OVERVIEW
Elaine C. Meyer, PhD, RN, MBE, FSSH is a nurse, clinical psychologist and ethicist with more than twenty-five years of experience in pediatric and neonatal intensive care settings. She is a founding member of the International PERCS Collaborative. Her teaching and academic work focuses on patient and family priorities and perspectives, healthcare conversations, everyday clinical ethics, and humanism in healthcare. To improve the emotional standard of care of patients and families, she has championed simulation-based educational learning to encourage clinicians, across disciplines and experience levels, be more direct, honest and confident. Her TEDx Talk, “On Being Present, Not Perfect” has over 75,000 views. She has published more than 125 peer-reviewed articles and chapters, and presents widely at national and international conferences.
BIOGRAPHY
Clinical Expertise and Innovation
Trained in nursing, clinical psychology and ethics, Dr. Meyer has worked for over twenty-five years in neonatal and pediatric critical care settings focusing on parental perspectives and priorities for care, end-of-life care, challenging conversations in healthcare, the ethics of everyday clinical encounters, and humanism in healthcare. Her clinical innovation and scholarship have enhanced the quality of family-provider communication and relationships, improved delivery of psychosocial services, and deepened the emotional standard of care. Her work has promoted meaningful clinical practice changes including visitation in critical care settings, parent presence during invasive procedures and resuscitation, and interprofessional teamwork. She co-developed and offered innovative parent retreats, entitled Reflecting on the Journey, for families of children and young adults diagnosed on the autism spectrum. Dr. Meyer's clinical work and scholarship in pediatric critical care and end-of-life care have contributed to understanding of parental perspectives and priorities to improve care and enhanced social support through psychosocial care delivery models, family conferences, and intimate bedside conversations. She has championed the priorities that families place on honest communication and trustworthy relationships, ready access to providers, emotional expression and support by providers, preservation of the integrity of the parent-child relationship, and integration of faith in clinical practice. She has been guided by the principles of empathic engagement, family-centered care, ethical integrity, and advocacy to effect meaningful cultural change addressing the problems and solutions as perceived by the patients and families themselves, rather than as hypothesized by professionals.
Teaching and Educational Leadership
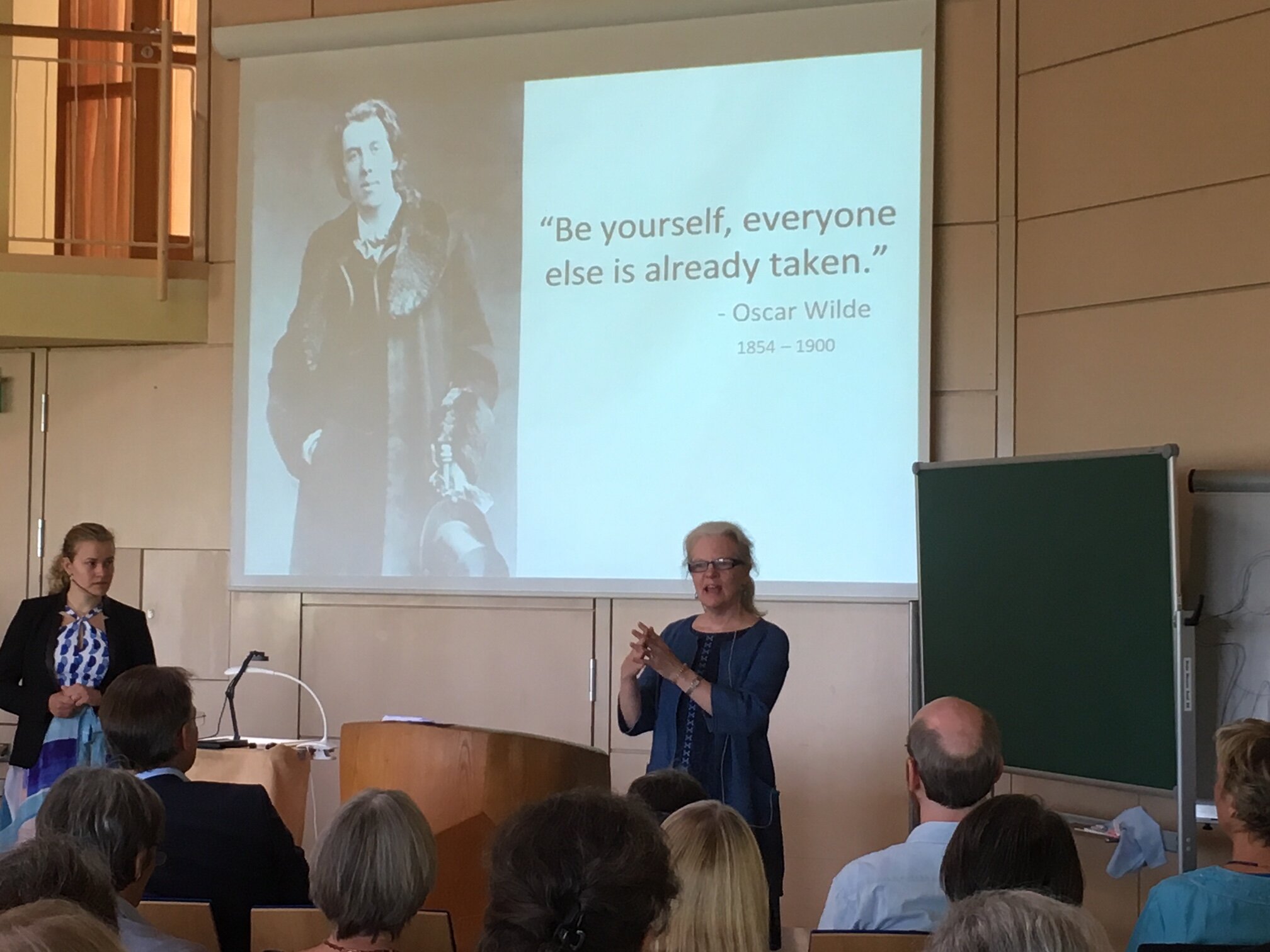
Dr. Meyer's teaching efforts have amplified her innovative clinical contributions. She serves as healthcare educational consultant at Fundación Garrahan in Buenos Aires, Argentina and senior scholar at the ARCIM Institute in Filderstadt, Germany. To improve communication and the emotional standard of care, she designed a simulation-based educational paradigm to encourage clinicians to be more honest, skillful and confident when engaging in challenging healthcare conversations. With colleagues, she successfully established the efficacy and cross-cultural applicability of the educational paradigm and workshops that have now been adapted to the fields of anesthesiology, neonatal and pediatric critical care, palliative care, radiology, general surgery, ophthalmology, and neurology. International workshop participants report long-term improvements in their preparation to hold difficult conversations, more confidence, enhanced communication and relational skills, and decreased anxiety. Challenging conversations include conveying serious diagnoses, informed consent, parent presence during invasive procedures and resuscitation, spirituality, organ donation, and disclosing adverse medical outcomes. Through the International PERCS Collaborative, her leadership has spawned programs in Italy, Australia, Germany, and Argentina. In 2018, she was inducted as a Fellow in the Society for Simulation in Healthcare. Currently, she serves as faculty member at the Center for Bioethics at Harvard Medical School. Dr. Meyer has been recognized with teaching awards for medical humanism, educational film production, and innovative scholarship in medical education.
Significant Supporting Activities
To promote dissemination of her work, Dr. Meyer has published more than 125 peer-reviewed articles and chapters, taught as Visiting Professor, and delivered keynote addresses at national and international conferences. To foster improved healthcare conversations and empathic engagement, and to educate worldwide, she delivered a successful TEDx Talk ‘On Being Present, Not Perfect’ that has exceeded 75,000 views. The Talk has been successfully incorporated into nursing and medical school curricula across the country and internationally. Through these innovative teaching efforts and social media platforms, the clinical and educational potential is limitless to improve challenging healthcare conversations and advance the emotional standard of care. Dr. Meyer also serves as a board member of Hope Hospice and Palliative Care in Rhode Island, and co-director of the Finding Joy in the Journey parent retreat for families with Autism Spectrum Disorder.
ELAINE ON HER TRAVELS
“Be yourself, everyone else is taken.”